A Comprehensive Description of the Anatomy and Histochemistry of Psychotria capillacea (Müll. Arg.) Standl. and an Investigation into Its Anti-Inflammatory Effects in Mice and Role in Scopolamine-Induced Memory Impairment
Abstract
:1. Introduction
2. Results
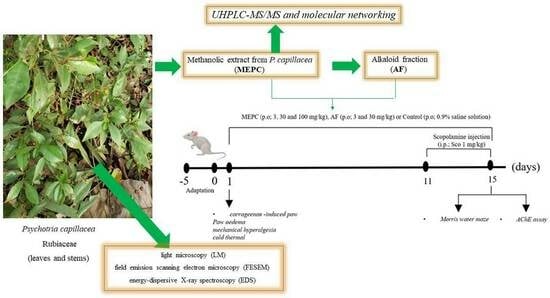
2.1. Micromorphology and Histochemistry Analysis
2.2. Chemical Composition
Molecular Networking
2.3. Anti-Inflammatory Activity
2.4. Learning and Memory Processes in Mice with Scopolamine (SCP)-Induced Dementia and AChE Inhibitory Activity
3. Discussion
4. Materials and Methods
4.1. Chemicals
4.2. Plant Material
4.3. Microscopy Procedure
4.4. Histochemical Analyses
4.5. Chemical Analyses
4.5.1. Extraction and Fractionation of the Methanolic Extract of P. capillacea
4.5.2. Chemical Analysis of MEPC by UHPLC—MS/MS, Molecular Networking and Alkaloidal Fraction (AF)
4.6. Animals
4.7. Anti-Inflammatory Activity
4.8. Neuroprotective Effects
Spatial Memory, Learning and AChE Inhibitory Activity
4.9. Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Formagio, A.S.N.; Volobuff, C.R.F.; Pereira, Z.V.; Vilela, L.O.; Vilegas, W. Coletânea Científica de Espécies de Psychotria (Rubiaceae): Florística e Aspectos Químicos e Farmacológicos; Atena Ponta Grossa: Ponta Grossa, Brazil, 2021; pp. 1–25. [Google Scholar] [CrossRef]
- Andersson, L.A. Provisional checklist of Neotropical Rubiaceae. Natl. Bot. Gard. Belg. 1992, 1, 1–9. [Google Scholar] [CrossRef]
- Formagio, A.S.N.; Volobuff, C.R.F.; Santiago, M.; Cardoso, C.L.A.; Vieira, M.C.; Pereira, Z.V.P. Evaluation of antioxidant activity, total flavonoids, tannins and phenolic compounds in Psychotria leaf extracts. Antioxidants 2014, 3, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Volobuff, C.R.F.; Oliveira Junior, P.C.; Santos, S.M.; Pereira, Z.F.; Ferreira, D.C.; Cardoso, C.A.L.; Ruiz, A.L.T.G.; Foglio, M.A.; de Carvalho, J.E.; Formagio, A.S.N. Antitumoral and anticholinesterasic activities of the seven species from Rubiaceae. Curr. Pharm. Biotechnol. 2019, 20, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Elisabetsky, E.; Castilhos, Z.C. Plants Used as Analgesics by Amazonian Caboclos as a Basis for Selecting Plants for Investigation. Int. J. Crude Drug Res. 1990, 28, 309–320. [Google Scholar] [CrossRef]
- Sutha, S.; Mohan, V.R.; Kumaresan, S.; Murugan, C.; Athiperumalsami, T. Ethnomedicinal plants used by the tribals of Kalakad-Mundanthurai Tiger Reserve (KMTR), Western Ghats, Tamil Nadu for the treatment of rheumatism. Indian J. Tradit. Know. 2010, 9, 502–509. [Google Scholar]
- Caballero-George, C.; Vanderheyden, P.M.; Solis, P.N.; Pieters, L.; Shahat, A.A.; Gupta, M.P.; Vauqueli, G.; Vlietinck, A.J. Biological screening of selected medicinal Panamanian plants by radioligand-binding techniques. Phytomedicine 2001, 8, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Armah, F.A.; Henneh, I.T.; Amponsah, I.K.; Biney, R.P.; Malcolm, F.; Alake, J.; Ahlidja, W.; Ahmed, M.A.; Adokoh, C.K.; Adukpo, G.E.; et al. Antidepressant and anxiolytic effects and subacute toxicity of the aerial parts of Psychotria ankasensis J.B.Hall (Rubiaceae) in murine models. Evid. Based Complement. Alternat. Med. 2021, 2021, 5543320. [Google Scholar] [CrossRef]
- de Carvalho, A.R.; De Carvalho, M.G.; Braz-Filho, R.; Vieira, I.J.C. Psychotria genus: Chemical constituents, biological activities, and synthetic studies. Stud. Nat. Prod. Chem. 2016, 48, 231–261. [Google Scholar] [CrossRef]
- Klein-Júnior, L.C.; Cretton, S.; Vander, H.Y.; Gasper, A.L.; Nejad-Ebrahimi, S.; Christen, P.; Henriques, A.T. Bioactive Azepine-Indole Alkaloids from Psychotria nemorosa. J. Nat. Prod. 2020, 83, 852–863. [Google Scholar] [CrossRef]
- Formagio, A.S.N.; Volobuff, C.R.F.; Kassuya, C.A.L.; Cardoso, C.A.L.; do Carmo Vieira, M.; Pereira, Z.V.; Bagatin, M.C.; Gauze, G.F. Psychotria leiocarpa extract and vincosamide reduce chemically-induced inflammation in mice and inhibit the acetylcholinesterase activity. Inflammation 2019, 42, 1561–1574. [Google Scholar] [CrossRef]
- de Carvalho, A.R.; Ferreira, R.O.; De Souza Passos, M.; Da Silva Boeno, S.I.; De Lima Glória Das Virgens, L.; Ventura, T.L.B.; Calixto, S.D.; Lassounskaia, E.; Carvalho, M.G.; Braz-Filho, R.; et al. Antimycobacterial and nitric oxide production inhibitory activities of triterpenes and alkaloids from Psychotria nuda (Cham. & Schltdl.) Wawra. Molecules 2019, 24, 1026. [Google Scholar] [CrossRef] [PubMed]
- Kirchweger, B.; Klein-Junior, L.C.; Pretsch, D.; Chen, Y.; Cretton, S.; Gasper, A.L.; Heyden, Y.V.; Christen, P.; Kirchmair, J.; Henriques, A.T.; et al. Azepine-indole alkaloids from Psychotria nemorosa modulate 5-HT2A receptors and prevent in vivo protein toxicity in transgenic Caenorhabditis elegans. Front. Neurosci. 2022, 16, 826289. [Google Scholar] [CrossRef] [PubMed]
- Tran, P.H.; Le, V.D.; Do, T.H.; Nguyen, T.L.; Nguyen, P.T.; Nguyen, T.T.; Nguyen, T.D. Anti-inflammatory constituents from Psychotria prainii H. Lév. Nat. Prod. Res. 2019, 33, 695–700. [Google Scholar] [CrossRef] [PubMed]
- Farias, F.M.; Passos, C.S.; Arbo, M.D.; Barros, D.M.; Gottfried, C.; Steffen, V.M.; Henriques, A.T. Strictosidinic acid, isolated from Psychotria myriantha Mull. Arg. (Rubiaceae), decreases serotonin levels in rat hippocampus. Fitoterapia 2012, 83, 1138–1143. [Google Scholar] [CrossRef]
- WHO—World Health Orgabuzation. Dementia. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 12 March 2024).
- Corbett, A.; Husebo, B.; Malcangio, M.; Staniland, A.; Cohen-Mansfield, J.; Aarsland, D.; Ballard, C. Assessment and treatment of pain in people with dementia. Nat. Rev. Neurol. 2012, 8, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Van Kooten, J.; Binnekade, T.T.; Wouden, J.C.V.; Stek, M.L.; Scherder, E.J.A.; Husebo, B.S.; Smalbrugge, M.; Hertogh, C.M.P.M. A review os pain prevalence in Alzheimer’s, vascular, frontotemporal and lewy body dementias. Dement. Geriatr. Cogn. Disord. 2016, 41, 220–232. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.J.; Meints, S.M.; Lazaridou, A.; Johnson, D.; Franceschelli, O.; Cornelius, M.; Schreiber, K.; Edwards, R.R. The effect of induced and chronic pain on attention. J. Pain 2019, 20, 1353–1361. [Google Scholar] [CrossRef] [PubMed]
- Morogiello, J.; Murray, N.G.; Hunt, T.N.; Harris, B.S.; Szekely, B.J.; Shaver, G.W. The effect of acute pain on executive function. J. Clin. Transl. Res. 2018, 4, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Mazza, S.; Frot, M.; Rey, A.E. A comprehensive literature review of chronic pain and memory. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 87, 183–192. [Google Scholar] [CrossRef]
- Moraes, T.M.S.; Rabelo, G.R.; Alexandrino, C.R.; Silva Neto, S.J.; Cunha, M. Comparative leaf anatomy and micromorphology of Psychotria species (Rubiaceae) from the Atlantic Rainforest. Acta Bot. Bras. 2011, 25, 178–190. [Google Scholar] [CrossRef]
- Miranda, O.F.; Souza, S.E.X.F.; Milan, R.J.; Bueno, A.B.; Almeida, M. Influence of environment on the leaf morpho-anatomy and histochemical of the ayahuasca leaf: Populations cultivated in extra-Amazonian regions. Acta Sci. 2020, 42, e50369. [Google Scholar] [CrossRef]
- Machado, C.D.; Santos, V.L.P.; Novak, R.S.; Koch, M.S.; Arcaro, G.; Raman, V.; Franco, C.R.C.; Farago, P.V.; Budel, J.M. Contributions of trichome micromorphology to the characterization of species traded as “Boldo”. Flora 2021, 279, 151827. [Google Scholar] [CrossRef]
- Raman, V.; Horner, H.T.; Khan, I.A. New and unusual forms of calcium oxalate raphide crystals in the plant kingdom. J. Plant Res. 2014, 127, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Santos, V.L.P.; Rodrigues, I.C.G.; Berté, R.; Raman, V.; Messias-Reason, I.J.; Budel, J.M. Review of Piper species growing in the Brazilian State of Paraná with emphasize on the vegetative anatomy and biological activities. Bot. Rev. 2021, 87, 23–54. [Google Scholar] [CrossRef]
- Budel, J.M.; Raman, V.; Monteiro, L.M.; Almeida, V.P.; Bobek, V.B.; Heiden, G.; Takeda, I.J.M.; Khan, I.A. Foliar anatomy and microscopy of six Brazilian species of Baccharis (Asteraceae). Microsc. Res. Tech. 2018, 81, 832–842. [Google Scholar] [CrossRef] [PubMed]
- Quinteiro, M.M.C.; Teixeira, D.C.; Moraes, M.G.; Silva, J.G. Anatomia foliar de Psychotria viridis Ruiz & Pav. (Rubiaceae). Rev. Univ. Rural. Série Ciências Vida 2006, 26, 30–41. [Google Scholar]
- Almeida, V.P.; Heiden, G.; Raman, V.; Novatski, A.; Bussade, J.E.; Farago, P.V.; Manfron, J. Microscopy and histochemistry of leaves and stems of Baccharis subgenus Coridifoliae (Asteraceae) through LM and SEM-EDS. Microsc. Microanal. 2021, 27, 1273–1289. [Google Scholar] [CrossRef]
- D’Almeida, W.; Monteiro, L.M.; Raman, V.; Rehman, J.U.; Paludo, K.S.; Maia, B.H.L.N.S.; Casapula, I.; Khan, I.A.; Farago, P.V.; Budel, J.M. Microscopy of Eugenia involucrata, chemical composition and biological activities of the volatile oil. Rev. Bras. Farmacogn. 2021, 31, 239–243. [Google Scholar] [CrossRef]
- Klider, L.M.; MacHado, C.D.; De Almeida, V.P.; Tirloni, C.A.S.; Marques, A.A.M.E.; Palozi, R.A.C.; Lorençone, B.R.; Romão, P.V.M.; Guarnier, L.P.; Casserino, N.S.; et al. Cuphea calophylla var. mesostemon (Koehne) S.A. Graham: A Whole-Ethnopharmacological Investigation. J. Med. Food 2021, 24, 394–410. [Google Scholar] [CrossRef]
- Lopes, K.S.; Marques, A.A.M.; Moreno, K.G.T.; Lorençone, B.R.; Leite, P.R.T.; da Silva, G.P.; Dos Santos, A.C.; Souza, R.I.C.; Gasparotto, F.M.; Cassemiro, N.S.; et al. Small conductance calcium-activated potassium channels and nitric oxide/cGMP pathway mediate cardioprotective effects of Croton urucurana Baill. In hypertensive rats. J. Ethnopharmacol. 2022, 293, 115255. [Google Scholar] [CrossRef]
- Pauzer, M.S.; Borsato, T.D.O.; de Almeida, V.P.; Raman, V.; Justus, B.; Pereira, C.B.; Flores, T.B.; Maia, B.H.L.N.S.; Meneghetti, E.K.; Kanunfre, E.C.; et al. Eucalyptus cinerea: Microscopic profile, chemical composition of essential oil and its antioxidant, microbiological and cytotoxic activities. Braz. Arch. Biol. Technol. 2021, 64, e21200772. [Google Scholar] [CrossRef]
- Ribeiro, M.A.S.; Gomes, C.M.B.; Formagio, A.S.N.; Pereira, Z.V.; Melo, U.Z.; Basso, E.A.; da Costa, W.F.; Baldoqui, D.C.; Sarragiotto, M.H. Structural characterization of dimeric indole alkaloids from Psychotria brachybotrya by NMR spectroscopy and theoretical calculations. Tetrahedron Lett. 2016, 57, 1331–1334. [Google Scholar] [CrossRef]
- Formagio, A.S.N.; Vilegas, W.; Volobuff, C.R.F.; Kassuya, C.A.L.; Almeida, V.P.; Manfron, J.; Pereira, Z.V.; Cabral, M.R.P.; Sarragiotto, M.H. Palicourea tomentosa (Aubl.) Borhidi: Microscopy, chemical composition and the analgesic, anti-inflammatory and anti-acetylcholinesterase potential. J. Ethnopharmacol. 2022, 291, 115050. [Google Scholar] [CrossRef] [PubMed]
- Das, M.; Balan, D.J.; Devi, K.P. Mitigation of oxidative stress with dihydroactinidiolide, a natural product against scopolamine-induced amnesia in Swiss albino mice. Neurotoxicology 2021, 86, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Jayawardena, T.U.; Kim, H.S.; Sanjeewa, K.K.A.; Han, E.J.; Jee, Y.; Ahn, G.; Rho, J.R.; Jeon, Y.J. Loliolide, isolated from Sargassum horneri; abate LPS-induced inflammation via TLR mediated NF-κB, MAPK pathways in macrophages. Algal Res. 2021, 56, 102297. [Google Scholar] [CrossRef]
- Oppong, M.B.; Cao, S.; Fang, S.M.; Amponsah, S.K.; Donkor, P.O.; Lartey, M.; Adutwum, L.A.; Opuni, K.F.M.; Zhao, F.; Feng, Q. In-vitro and in-vivo anti-inflammatory properties of extracts and isolates of Pangdahai. Phytomed. Plus 2024, 4, 100533. [Google Scholar] [CrossRef]
- Lomba, L.A.; Vogt, P.H.; Souza, V.E.P.; Leite-Avalca, M.C.G.; Verdan, M.H.; Stefanello, M.E.A.; Zampronio, A.R. A Naphthoquinone from Sinningia canescens Inhibits Inflammation and Fever in Mice. Inflammation 2017, 40, 1051–1061. [Google Scholar] [CrossRef] [PubMed]
- Broeke, E.N.; Mouraux, A.; Groneberg, A.; Pfau, D.B.; Treede, R.D.; Klein, T. Characterizing pinprick-evoked brain potentials before and after experimentally induced secondary hyperalgesia. J. Neurophysiol. 2015, 114, 2672–2681. [Google Scholar] [CrossRef] [PubMed]
- Maracle, E.C.; Hung, L.Y.; Fell, S.I.; Osmond, M.R.; Brown, S.H.M.; Srbely, J.Z. A Comparison of the Sensitivity of Brush Allodynia and Semmes-Weinstein Monofilament Testing in the Detection of Allodynia Within Regions of Secondary Hyperalgesia in Humans. Pain Pract. 2017, 17, 16–24. [Google Scholar] [CrossRef]
- Deuis, J.R.; Dvorakova, L.S.; Vetter, I. Methods used to evaluate pain behaviors in rodents. Front. Mol. Neurosci. 2017, 10, 284. [Google Scholar] [CrossRef]
- Calixto, N.O.; Cordeiro, M.S.; Giorno, T.B.S.; Oliveira, G.G.; Lopes, N.P.; Fernandes, P.D.; Pinto, A.C.; Rezende, C.M. Chemical constituents of Psychotria nemorosa Gardner and antinociceptive activity. J. Braz. Chem. Soc. 2017, 28, 707–723. [Google Scholar] [CrossRef]
- Leal, M.B.; Elisabetsky, E. Opioid-like activity of Psychotria brachypoda. Int. J. Pharmacol. 1996, 34, 267–272. [Google Scholar] [CrossRef]
- Elisabetsky, E.; Amador, T.A.; Albuquerque, R.R.; Nunes, D.S.; Carvalho, A.C.T. Analgesic activity of Psychotria colorata (Willd. ex R. & S.) Muell. Arg. Alkaloids. J. Ethnopharmac. 1995, 48, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Passos, C.S.; Simões-Pires, C.A.; Nurisso, A.; Soldi, T.C.; Kato, L.; De Oliveira, C.M.A.; Faria, E.O.; Marcourt, L.; Gottfried, C.; Pierre-Alain Carrupt, P.A.; et al. Indole alkaloids of Psychotria as multifunctional cholinesterases and monoamine oxidases inhibitors. Phytochemistry 2013, 86, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Both, F.L.; Meneghini, L.; Kerber, V.A.; Henriques, A.T.; Elisabetsky, E. Role of glutamate and dopamine receptors in the psychopharmacological profile of the indole alkaloid psychollatine. J. Nat. Prod. 2006, 69, 342–345. [Google Scholar] [CrossRef] [PubMed]
- Farias, F.M.; Passos, C.S.; Arbo, M.D.; Zuanazzi, J.A.; Steffen, V.M.; Henriques, A.T. Monoamine levels in rat striatum after acute intraperitoneal injection of strictosidinic acid isolated from Psychotria myriantha Mull. Arg. (Rubiaceae). Phytomedicine 2010, 17, 289–291. [Google Scholar] [CrossRef] [PubMed]
- Both, F.L.; Meneghini, L.; Kerber, V.A.; Henriques, A.T.; Elisabetsky, E. Psychopharmacological profile of the alkaloid psychollatine as a 5HT2A/C serotonin modulator. J. Nat. Prod. 2005, 68, 374–380. [Google Scholar] [CrossRef]
- Brito, P.S.; Sabedotti, C.; Flores, T.B.; Raman, V.; Bussade, J.E.; Farago, P.V.; Manfron, J. Light and scanning electron microscopy, energy dispersive X-ray spectroscopy and histochemistry of Eucalyptus tereticornis. Microsc. Microanal. 2021, 27, 1295–1303. [Google Scholar] [CrossRef]
- Johansen, D.A. Plant Microtechnique; Mc Graw Hill Book: New York, NY, USA, 1940. [Google Scholar]
- Furr, M.; Mahlberg, P.G. Histochemical analyses of laticifers and glandular trichomes in Cannabis sativa. J. Nat. Prod. 1981, 44, 153–159. [Google Scholar] [CrossRef]
- Yoder, L.R.; Mahlberg, P.G. Reactions of alkaloid and histochemical indicators in laticifers and specialized parenchyma cells of Catharanthus roseus (Apocynaceae). Am. J. Bot. 1976, 63, 1167–1173. [Google Scholar] [CrossRef]
- Gabe, M. Techniques Histologiques; Masson Cie: Paris, France, 1968. [Google Scholar]
- Pearse, A.G.E. Histochemistry: Theoretical and Applied, 3rd ed.; The Williams & Wilkins Company: Baltimore, MD, USA, 1972. [Google Scholar]
- Allen, F.; Greiner, R.; Wishart, D. Competitive fragmentation modeling of ESI-MS/MS spectra for putative metabolite identification. Metabolomics 2015, 11, 98–110. [Google Scholar] [CrossRef]
- He, D.D.; Wu, H.; Wei, Y.; Liu, W.; Huang, F.; Shi, H.L.; Zhang, B.B.; Wu, X.J.; Wang, C.H. Effects of harmine, an acetylcholinesterase inhibitor, on spatial learning and memory of APP/PS1 transgenic mice and scopolamine-induced memory impairment mice. Eur. J. Pharmacol. 2015, 768, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Bradford, M.M. A rapid and sensitive method for quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 1976, 72, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Ellman, G.L.; Courtney, K.D.; Valentino, A.J.; Featherstone, R.M. A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem. Pharmacol. 1961, 7, 88–95. [Google Scholar] [CrossRef] [PubMed]









| Compounds | tr/ min | Molecular Formula | m/z | Ion Precursor m/z | Error/ ppm | MS/MS |
|---|---|---|---|---|---|---|
| vincanol (PC-1) | 0.97 | C19H24N2O [M + Na]+ | 319.1786 | 319.1814 | 8.77 | 160; 142; 98 |
| vomifoliol (PC-2) | 4.44 | C13H20NaO3 [M + H-H20]+ | 207.1384 | 207.1348 | 7.37 | 149; 131; 115; 105; 91; 79 |
| loliolide (PC-3) | 4.66 | C11H17O3 [M + H]+ | 197.1172 | 197.1140 | 6.23 | 162; 149; 133; 117; 105; 89 |
| vincosamide (PC-4) | 4.74 | C26H30N2O8 [M + H]+ | 499.2075 | 499.2002 | 4.62 | 337; 267; 171; 144 |
| dihydroactinidiolide (PC-5) | 5.42 | C11H17O2 [M + H]+ | 181.1223 | 181.1193 | 6.56 | 145; 135; 121; 93 |
| N,N,N-trimethyltryptamine (PC-6) | 5.55 | C13H19N2 [M + NH4]+ | 221.1887 | 221.1864 | 7.20 | 161; 147; 133; 119; 105; 91; 81 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Formagio, A.S.N.; Vilegas, W.; Kassuya, C.A.L.; De Almeida, V.P.; Manfron, J.; Konkiewitz, E.C.; Ziff, E.B.; Faoro, J.A.M.; Dos Santos, J.M.; Cecatto, A.J.; et al. A Comprehensive Description of the Anatomy and Histochemistry of Psychotria capillacea (Müll. Arg.) Standl. and an Investigation into Its Anti-Inflammatory Effects in Mice and Role in Scopolamine-Induced Memory Impairment. Pharmaceuticals 2024, 17, 564. https://doi.org/10.3390/ph17050564
Formagio ASN, Vilegas W, Kassuya CAL, De Almeida VP, Manfron J, Konkiewitz EC, Ziff EB, Faoro JAM, Dos Santos JM, Cecatto AJ, et al. A Comprehensive Description of the Anatomy and Histochemistry of Psychotria capillacea (Müll. Arg.) Standl. and an Investigation into Its Anti-Inflammatory Effects in Mice and Role in Scopolamine-Induced Memory Impairment. Pharmaceuticals. 2024; 17(5):564. https://doi.org/10.3390/ph17050564
Chicago/Turabian StyleFormagio, Anelise Samara Nazari, Wagner Vilegas, Cândida Aparecida Leite Kassuya, Valter Paes De Almeida, Jane Manfron, Elisabete Castelon Konkiewitz, Edward Benjamin Ziff, Janaine Alberto Marangoni Faoro, Jessica Maurino Dos Santos, Ana Julia Cecatto, and et al. 2024. "A Comprehensive Description of the Anatomy and Histochemistry of Psychotria capillacea (Müll. Arg.) Standl. and an Investigation into Its Anti-Inflammatory Effects in Mice and Role in Scopolamine-Induced Memory Impairment" Pharmaceuticals 17, no. 5: 564. https://doi.org/10.3390/ph17050564